Allergy
About this schools Wikipedia selection
SOS Children volunteers helped choose articles and made other curriculum material To compare sponsorship charities this is the best sponsorship link.
| Allergy | |
|---|---|
| Classification and external resources | |
| ICD- 10 | T 78.4 |
| ICD- 9 | 995.3 |
| DiseasesDB | 33481 |
| MedlinePlus | 000812 |
| eMedicine | med/1101 |
| MeSH | D006967 |
Allergy is a disorder of the immune system often also referred to as atopy. Allergic reactions occur to environmental substances known as allergens; these reactions are acquired, predictable and rapid. Strictly, allergy is one of four forms of hypersensitivity and is called type I (or immediate) hypersensitivity. It is characterized by excessive activation of certain white blood cells called mast cells and basophils by a type of antibody known as IgE, resulting in an extreme inflammatory response. Common allergic reactions include eczema, hives, hay fever, asthma, food allergies, and reactions to the venom of stinging insects such as wasps and bees.
Mild allergies like hay fever are highly prevalent in the human population and cause symptoms such as allergic conjunctivitis, itchiness, and runny nose. Allergies can play a major role in conditions such as asthma. In some people, severe allergies to environmental or dietary allergens or to medication may result in life-threatening anaphylactic reactions and potentially death.
A variety of tests now exist to diagnose allergic conditions; these include testing the skin for responses to known allergens or analyzing the blood for the presence and levels of allergen-specific IgE. Treatments for allergies include allergen avoidance, use of anti-histamines, steroids or other oral medications, immunotherapy to desensitize the response to allergen, and targeted therapy.
Classification and history
The concept "allergy" was originally introduced in 1906 by the Viennese pediatrician Clemens von Pirquet, after he noted that some of his patients were hypersensitive to normally innocuous entities such as dust, pollen, or certain foods. Pirquet called this phenomenon "allergy" from the Greek words allos meaning "other" and ergon meaning "work". Historically, all forms of hypersensitivity were classified as allergies, and all were thought to be caused by an improper activation of the immune system. Later, it became clear that several different disease mechanisms were implicated, with the common link to a disordered activation of the immune system. In 1963, a new classification scheme was designed by Philip Gell and Robin Coombs that described four types of hypersensitivity reactions, known as Type I to Type IV hypersensitivity. With this new classification, the word "allergy" was restricted to only type I hypersensitivities (also called immediate hypersensitivity), which are characterized as rapidly developing reactions.
A major breakthrough in understanding the mechanisms of allergy was the discovery of the antibody class labeled immunoglobulin E (IgE) - Kimishige Ishizaka and co-workers were the first to isolate and describe IgE in the 1960s.
Signs and symptoms
| Affected organ | Symptom |
|---|---|
| Nose | swelling of the nasal mucosa (allergic rhinitis) |
| Sinuses | allergic sinusitis |
| Eyes | redness and itching of the conjunctiva (allergic conjunctivitis) |
| Airways | Sneezing, coughing, bronchoconstriction, wheezing and dyspnea, sometimes outright attacks of asthma, in severe cases the airway constricts due to swelling known as angioedema |
| Ears | feeling of fullness, possibly pain, and impaired hearing due to the lack of eustachian tube drainage. |
| Skin | rashes, such as eczema and hives (urticaria) |
| Gastrointestinal tract | abdominal pain, bloating, vomiting, Diarrhea |
Many allergens, such as dust or pollen, are airborne particles. In these cases, symptoms arise in areas in contact with air, such as eyes, nose and lungs. For instance, allergic rhinitis, also known as hay fever, causes irritation of the nose, sneezing, and itching and redness of the eyes. Inhaled allergens can also lead to asthmatic symptoms, caused by narrowing of the airways ( bronchoconstriction) and increased production of mucus in the lungs, shortness of breath ( dyspnea), coughing and wheezing.
Aside from these ambient allergens, allergic reactions can result from foods, insect stings, and reactions to medications like aspirin and antibiotics such as penicillin. Symptoms of food allergy include abdominal pain, bloating, vomiting, diarrhoea, itchy skin, and swelling of the skin during hives. Food allergies rarely cause respiratory (asthmatic) reactions, or rhinitis. Insect stings, antibiotics, and certain medicines produce a systemic allergic response that is also called anaphylaxis; multiple organ systems can be affected, including the digestive system, the respiratory system, and the circulatory system. Depending of the rate of severity, it can cause cutaneous reactions, bronchoconstriction, edema, hypotension, coma, and even death. This type of reaction can be triggered suddenly, or the onset can be delayed. The severity of this type of allergic response often requires injections of epinephrine, sometimes through a device known as the Epi-Pen auto-injector. The nature of anaphylaxis is such that the reaction can seem to be subsiding, but may recur throughout a prolonged period of time.
Substances that come into contact with the skin, such as latex, are also common causes of allergic reactions, known as contact dermatitis or eczema. Skin allergies frequently cause rashes, or swelling and inflammation within the skin, in what is known as a " wheal and flare" reaction characteristic of hives and angioedema.
Cause
Risk factors for allergy can be placed in two general categories, namely host and environmental factors. Host factors include heredity, sex, race, and age, with heredity being by far the most significant. There have been recent increases in the incidence of allergic disorders, however, that cannot be explained by genetic factors alone. The four main environmental candidates are alterations in exposure to infectious diseases during early childhood, environmental pollution, allergen levels, and dietary changes.
Genetic basis
Allergic diseases are strongly familial: identical twins are likely to have the same allergic diseases about 70% of the time; the same allergy occurs about 40% of the time in non-identical twins. Allergic parents are more likely to have allergic children, and their allergies are likely to be more severe than those from non-allergic parents. Some allergies, however, are not consistent along genealogies; parents who are allergic to peanuts may have children who are allergic to ragweed. It seems that the likelihood of developing allergies is inherited and related to an irregularity in the immune system, but the specific allergen is not.
The risk of allergic sensitization and the development of allergies varies with age, with young children most at risk. Several studies have shown that IgE levels are highest in childhood and fall rapidly between the ages of 10 and 30 years. The peak prevalence of hay fever is highest in children and young adults and the incidence of asthma is highest in children under 10. Overall, boys have a higher risk of developing allergy than girls, although for some diseases, namely asthma in young adults, females are more likely to be affected. Sex differences tend to decrease in adulthood. Ethnicity may play a role in some allergies, however racial factors have been difficult to separate from environmental influences and changes due to migration. Interestingly, it has been suggested that different genetic loci are responsible for asthma, specifically, in people of Caucasian, Hispanic, Asian, and African origins.
Environmental factors
International differences have been associated with the number of individuals within a population that suffer from allergy. Allergic diseases are more common in industrialized countries than in countries that are more traditional or agricultural, and there is a higher rate of allergic disease in urban populations versus rural populations, although these differences are becoming less defined.
Exposure to allergens, especially in early life, is an important risk factor for allergy. Alterations in exposure to microorganisms is the most plausible explanation, at present, for the increase in atopic allergy. Since children that live in large families or overcrowded households, or attend day care, have a reduced incidence of allergic disease, a relationship has been proposed between exposures to bacteria and viruses during childhood, and protection against the development of allergy, which has been called – the " hygiene hypothesis". Exposure to endotoxin and other components of bacteria may reduce atopic diseases. Endotoxin exposure reduces release of inflammatory cytokines such as TNF-α, IFNγ, interleukin-10, and interleukin-12 from white blood cells ( leukocytes) that circulate in the blood. Certain microbe-sensing proteins, known as Toll-like receptors, found on the surface of cells in the body are also thought to be involved in these processes.
Gutworms and similar parasites are present in untreated drinking water in developing countries, and were present in the water of developed countries until the routine chlorination and purification of drinking water supplies. Recent research has shown that some common parasites, such as intestinal worms (e.g. hookworms), secrete chemicals into the gut wall (and hence the bloodstream) that suppress the immune system and prevent the body from attacking the parasite. This gives rise to a new slant on the hygiene hypothesis theory — that co-evolution of man and parasites has led to an immune system that only functions correctly in the presence of the parasites. Without them, the immune system becomes unbalanced and oversensitive. In particular, research suggests that allergies may coincide with the delayed establishment of gut flora in infants. However, the research to support this theory is conflicting, with some studies performed in China and Ethiopia showing an increase in allergy in people infected with intestinal worms. Clinical trials have been initiated to test the effectiveness of certain worms in treating some allergies. It may be that the term 'parasite' could turn out to be inappropriate, and in fact a hitherto unsuspected symbiosis is at work. For more information on this topic, see Helminthic therapy.
Pathophysiology
The pathophysiology of allergic responses can be divided into two phases. The first is an acute response that occurs immediately after exposure to an allergen. This phase can either subside or progress into a "late phase reaction" which can substantially prolong the symptoms of a response, and result in tissue damage.
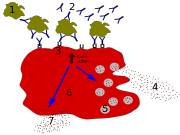
Acute response
In the early stages of allergy, a type I hypersensitivity reaction against an allergen, encountered for the first time, causes a response in a type of immune cell called a TH2 lymphocyte, which belongs to a subset of T cells that produce a cytokine called interleukin-4 (IL-4). These TH2 cells interact with other lymphocytes called B cells, whose role is production of antibodies. Coupled with signals provided by IL-4, this interaction stimulates the B cell to begin production of a large amount of a particular type of antibody known as IgE. Secreted IgE circulates in the blood and binds to an IgE-specific receptor (a kind of Fc receptor called FcεRI) on the surface of other kinds of immune cells called mast cells and basophils, which are both involved in the acute inflammatory response. The IgE-coated cells, at this stage are sensitized to the allergen.
If later exposure to the same allergen occurs, the allergen can bind to the IgE molecules held on the surface of the mast cells or basophils. Cross-linking of the IgE and Fc receptors occurs when more than one IgE-receptor complex interacts with the same allergenic molecule, and activates the sensitized cell. Activated mast cells and basophils undergo a process called degranulation, during which they release histamine and other inflammatory chemical mediators ( cytokines, interleukins, leukotrienes, and prostaglandins) from their granules into the surrounding tissue causing several systemic effects, such as vasodilation, mucous secretion, nerve stimulation and smooth muscle contraction. This results in rhinorrhea, itchiness, dyspnea, and anaphylaxis. Depending on the individual, allergen, and mode of introduction, the symptoms can be system-wide (classical anaphylaxis), or localized to particular body systems; asthma is localized to the respiratory system and eczema is localized to the dermis.
Late-phase response
After the chemical mediators of the acute response subside, late phase responses can often occur. This is due to the migration of other leukocytes such as neutrophils, lymphocytes, eosinophils and macrophages to the initial site. The reaction is usually seen 2-24 hours after the original reaction. Cytokines from mast cells may also play a role in the persistence of long-term effects. Late phase responses seen in asthma are slightly different from those seen in other allergic responses, although they are still caused by release of mediators from eosinophils, and are still dependent on activity of TH2 cells.
Diagnosis
Before a diagnosis of allergic disease can be confirmed, the other possible causes of the presenting symptoms should be carefully considered. Vasomotor rhinitis, for example, is one of many maladies that shares symptoms with allergic rhinitis, underscoring the need for professional differential diagnosis. Once a diagnosis of asthma, rhinitis, anaphylaxis, or other allergic disease has been made, there are several methods for discovering the causative agent of that allergy.
Skin testing
For assessing the presence of allergen-specific IgE antibodies, allergy skin testing is preferred over blood allergy tests because it is more sensitive and specific, simpler to use, and less expensive. Skin testing is also known as "puncture testing" and "prick testing" due to the series of tiny puncture or pricks made into the patient's skin. Small amounts of suspected allergens and/or their extracts (pollen, grass, mite proteins, peanut extract, etc.) are introduced to sites on the skin marked with pen or dye (the ink/dye should be carefully selected, lest it cause an allergic response itself). A small plastic or metal device is used to puncture or prick the skin. Sometimes, the allergens are injected "intradermally" into the patient's skin, with a needle and syringe. Common areas for testing include the inside forearm and the back. If the patient is allergic to the substance, then a visible inflammatory reaction will usually occur within 30 minutes. This response will range from slight reddening of the skin to a full-blown hive (called "wheal and flare") in more sensitive patients. Interpretation of the results of the skin prick test is normally done by allergists on a scale of severity, with +/- meaning borderline reactivity, and 4+ being a large reaction. Increasingly, allergists are measuring and recording the diameter of the wheal and flare reaction. Interpretation by well-trained allergists is often guided by relevant literature. Some patients may believe they have determined their own allergic sensitivity from observation, but a skin test has been shown to be much better than patient observation to detect allergy.
If a serious life threatening anaphylactic reaction has brought a patient in for evaluation, some allergists will prefer an initial blood test prior to performing the skin prick test. Skin tests may not be an option if the patient has widespread skin disease or has taken antihistamines sometime the last several days.
Blood testing
Various blood allergy testing methods are also available for detecting allergy to specific substances. This kind of testing measures a "total IgE level" - an estimate of IgE contained within the patient's serum. This can be determined through the use of radiometric and colormetric immunoassays. Radiometric assays include the radioallergosorbent test (RAST) test method, which uses IgE-binding (anti-IgE) antibodies labeled with radioactive isotopes for quantifying the levels of IgE antibody in the blood. Other newer methods use colorimetric or fluorometric technology in the place of radioactive isotopes. Some "screening" test methods are intended to provide qualitative test results, giving a "yes" or "no" answer in patients with suspected allergic sensitization. One such method has a sensitivity of about 70.8% and a positive predictive value of 72.6% according to a large study.
A low total IgE level is not adequate to rule out sensitization to commonly inhaled allergens. Statistical methods, such as ROC curves, predictive value calculations, and likelihood ratios have been used to examine the relationship of various testing methods to each other. These methods have shown that patients with a high total IgE have a high probability of allergic sensitization, but further investigation with specific allergy tests for a carefully chosen allergens is often warranted.
Treatment
There have been enormous improvements in the medical treatments used to treat allergic conditions. With respect to anaphylaxis and hypersensitivity reactions to foods, drugs, and insects and in allergic skin diseases, advances have included the identification of food proteins to which IgE binding is associated with severe reactions and development of low-allergen foods, improvements in skin prick test predictions; evaluation of the atopy patch test; in wasp sting outcomes predictions and a rapidly disintegrating epinephrine tablet, and anti-IL-5 for eosinophilic diseases.
Traditionally treatment and management of allergies involved simply avoiding the allergen in question or otherwise reducing exposure. For instance, people with cat allergies were encouraged to avoid them. While avoidance may help to reduce symptoms and avoid life-threatening anaphylaxis, it is difficult to achieve for those with pollen or similar air-borne allergies. Strict avoidance still has a role in management though, and is often used in managing food allergies.
Pharmacotherapy
Several antagonistic drugs are used to block the action of allergic mediators, or to prevent activation of cells and degranulation processes. These include antihistamines, cortisone, dexamethasone, hydrocortisone, epinephrine (adrenaline), theophylline and cromolyn sodium. Anti- leukotrienes, such as Montelukast (Singulair) or Zafirlukast (Accolate), are FDA approved for treatment of allergic diseases. Anti- cholinergics, decongestants, mast cell stabilizers, and other compounds thought to impair eosinophil chemotaxis, are also commonly used. These drugs help to alleviate the symptoms of allergy, and are imperative in the recovery of acute anaphylaxis, but play little role in chronic treatment of allergic disorders.
Immunotherapy
Desensitization or hyposensitization is a treatment in which the patient is gradually vaccinated with progressively larger doses of the allergen in question. This can either reduce the severity or eliminate hypersensitivity altogether. It relies on the progressive skewing of IgG antibody production, to block excessive IgE production seen in atopys. In a sense, the person builds up immunity to increasing amounts of the allergen in question. Studies have demonstrated the long-term efficacy and the preventive effect of immunotherapy in reducing the development of new allergy. Meta-analyses have also confirmed efficacy of the treatment in allergic rhinitis in children and in asthma. A review by the Mayo Clinic in Rochester confirmed the safety and efficacy of allergen immunotherapy for allergic rhinitis and conjunctivitis, allergic forms of asthma, and stinging insect based on numerous well-designed scientific studies. Additionally, national and international guidelines confirm the clinical efficacy of injection immunotherapy in rhinitis and asthma, as well as the safety, provided that recommendations are followed.
A second form of immunotherapy involves the intravenous injection of monoclonal anti-IgE antibodies. These bind to free and B-cell associated IgE; signalling their destruction. They do not bind to IgE already bound to the Fc receptor on basophils and mast cells, as this would stimulate the allergic inflammatory response. The first agent of this class is Omalizumab. While this form of immunotherapy is very effective in treating several types of atopy, it should not be used in treating the majority of people with food allergies.
A third type, Sublingual immunotherapy, is an orally-administered therapy which takes advantage of oral immune tolerance to non-pathogenic antigens such as foods and resident bacteria. This therapy currently accounts for 40 percent of allergy treatment in Europe. In the United States, sublingual immunotherapy is gaining support among traditional allergists and is endorsed by doctors who treat allergy.
Unproven or ineffective treatments
An experimental treatment, enzyme potentiated desensitization (EPD), has been tried for decades but is not generally accepted as effective. EPD uses dilutions of allergen and an enzyme, beta-glucuronidase, to which T-regulatory lymphocytes are supposed to respond by favouring desensitization, or down-regulation, rather than sensitization. EPD has also been tried for the treatment of autoimmune diseases but again is not FDA approved or of proven effectiveness.
In alternative medicine, a number of allergy treatments are described by its practitioners, particularly naturopathic, herbal medicine, homeopathy, traditional Chinese medicine and kinesiology. Systematic literature searches conducted by the Mayo Clinic through 2006, involving hundreds of articles studying multiple conditions, including asthma and upper respiratory tract infection showed no effectiveness of any alternative treatments, and no difference compared with placebo. The authors concluded that, based on rigorous clinical trials of all types of homeopathy for childhood and adolescence ailments, there is no convincing evidence that supports the use of alternative treatments.
Epidemiology
Many diseases related to inflammation such as type 1 diabetes, rheumatoid arthritis and allergic diseases—hay fever and asthma—have increased in the Western world over the past 2-3 decades. Rapid increases in allergic asthma and other atopic disorders in industrialized nations probably began in the 1960s and 1970s, with further increases occurring during the 1980s and 1990s, although some suggest that a steady rise in sensitization has been occurring since the 1920s. The incidence of atopy in developing countries has generally remained much lower.
| Allergy type | United States | United Kingdom |
|---|---|---|
| Allergic rhinitis | 35.9 million (about 11% of the population) | 3.3 million (about 5.5% of the population) |
| Asthma | 10 million suffer from allergic asthma (about 3% of the population). The prevalence of asthma increased 75% from 1980-1994. Asthma prevalence is 39% higher in African Americans than in Anglo Saxons. | 5.7 million (about 9.4%). In six and seven year olds asthma increased from 18.4% to 20.9% over five years, during the same time the rate decreased from 31% to 24.7% in 13 to 14 year olds. |
| Atopic eczema | About 9% of the population. Between 1960 and 1990 prevalence has increased from 3% to 10% in children. | 5.8 million (about 1% severe). |
| Anaphylaxis | At least 40 deaths per year due to insect venom. About 400 deaths due to penicillin anaphylaxis. About 220 cases of anaphylaxis and 3 deaths per year are due to latex allergy. An estimated 150 people die annually from anaphylaxis due to food allergy. | Between 1999 and 2006, 48 deaths occurred in people ranging from five months to 85 years old. |
| Insect venom | Around 15% of adults have mild, localized allergic reactions. Systemic reactions occur in 3% of adults and less than 1% of children. | Unknown |
| Drug allergies | Anaphylactic reactions to penicillin cause 400 deaths. | Unknown |
| Food allergies | 2-4% of children and 1-2% of adults. Peanut and/or tree nut (e.g. walnut, almond and cashew) allergy affects about three million Americans, or 1.1% of the population. | 5-7% of infants and 1-2% of adults. A 117.3% increase in peanut allergies was observed from 2001 to 2005, an estimated 25,700 people in England are affected. |
| Multiple allergies (Asthma, eczema and allergic rhinitis together) |
? | 2.3 million (about 3.7%), prevalence has increased by 48.9% between 2001 and 2005. |
Although genetic factors fundamentally govern susceptibility to atopic disease, increases in atopy have occurred within too short a time frame to be explained by a genetic change in the population, thus pointing to environmental or lifestyle changes. Several hypotheses have been identified to explain this increased prevalence; increased exposure to perennial allergens due to housing changes and increasing time spent indoors, and changes in cleanliness or hygiene that have resulted in the decreased activation of a common immune control mechanism, coupled with dietary changes, obesity and decline in physical exercise. The hygiene hypothesis maintains that high living standards and hygienic conditions exposes children to fewer infections. It is thought that reduced bacterial and viral infections early in life direct the maturing immune system away from TH1 type responses, leading to unrestrained TH2 responses that allow for an increase in allergy.
Changes in rates and types of infection alone however, have been unable to explain the observed increase in allergic disease, and recent evidence has focused attention on the importance of the gastrointestinal microbial environment. Evidence has shown that exposure to food and fecal-oral pathogens, such as hepatitis A, Toxoplasma gondii, and Helicobacter pylori (which also tend to be more prevalent in developing countries), can reduce the overall risk of atopy by more than 60%, and an increased prevalence of parasitic infections has been associated with a decreased prevalence of asthma. It is speculated that these infections exert their effect by critically altering TH1/TH2 regulation. Important elements of newer hygiene hypotheses also include exposure to endotoxins, exposure to pets and growing up on a farm.
Medical specialty
In the United States physicians who hold certification by the American Board of Allergy and Immunology (ABAI) have successfully completed an accredited educational program and an evaluation process, including a secure, proctored examination to demonstrate the knowledge, skills, and experience to the provision of patient care in allergy and immunology. An allergist-immunologist is a physician specially trained to manage and treat asthma and the other allergic diseases. Becoming an allergist-immunologist requires completion of at least nine years of training. After completing medical school and graduating with a medical degree, a physician will then undergo three years of training in internal medicine (to become an internist) or pediatrics (to become a pediatrician). Once physicians have finished training in one of these specialties, they must pass the exam of either the American Board of Pediatrics (ABP) or the American Board of Internal Medicine (ABIM). Internists or pediatricians who wish to focus on the sub-specialty of allergy-immunology then complete at least an additional two years of study, called a fellowship, in an allergy-immunology training program. Allergist-immunologists who are listed as ABAI-certified have successfully passed the certifying examination of the American Board of Allergy and Immunology (ABAI), following their fellowship.
In the United Kingdom, allergy is a subspecialty of general medicine or pediatrics. After obtaining postgraduate exams ( MRCP or MRCPCH respectively) a doctor works as several years as a specialist registrar before qualifying for the General Medical Council specialist register. Allergy services may also be delivered by immunologists. A 2003 Royal College of Physicians report presented a case for improvement of what were felt to be inadequate allergy services in the UK. In 2006, the House of Lords convened a subcommittee that reported in 2007. It concluded likewise that allergy services were insufficient to deal with what the Lords referred to as an "allergy epidemic" and its social cost; it made several other recommendations.