Multiple sclerosis
Background to the schools Wikipedia
SOS Children produced this website for schools as well as this video website about Africa. SOS Children works in 45 African countries; can you help a child in Africa?
Multiple sclerosis (MS), also known as "disseminated sclerosis" or "encephalomyelitis disseminata", is an inflammatory disease in which the fatty myelin sheaths around the axons of the brain and spinal cord are damaged, leading to demyelination and scarring as well as a broad spectrum of signs and symptoms. Disease onset usually occurs in young adults, and it is more common in women. It has a prevalence that ranges between 2 and 150 per 100,000. MS was first described in 1868 by Jean-Martin Charcot.
MS affects the ability of nerve cells in the brain and spinal cord to communicate with each other effectively. Nerve cells communicate by sending electrical signals called action potentials down long fibers called axons, which are contained within an insulating substance called myelin. In MS, the body's own immune system attacks and damages the myelin. When myelin is lost, the axons can no longer effectively conduct signals. The name multiple sclerosis refers to scars (sclerae-—better known as plaques or lesions) particularly in the white matter of the brain and spinal cord, which is mainly composed of myelin. Although much is known about the mechanisms involved in the disease process, the cause remains unknown. Theories include genetics or infections. Different environmental risk factors have also been found.
Almost any neurological symptom can appear with the disease, and the disease often progresses to physical and cognitive disability. MS takes several forms, with new symptoms occurring either in discrete attacks (relapsing forms) or accumulating over time (progressive forms). Between attacks, symptoms may go away completely, but permanent neurological deficits often occur, especially as the disease advances.
There is no known cure for multiple sclerosis. Treatments attempt to return function after an attack, prevent new attacks, and prevent disability. MS medications can have adverse effects or be poorly tolerated, and many people pursue alternative treatments, despite the lack of supporting scientific study. The prognosis is difficult to predict; it depends on the subtype of the disease, the individual's disease characteristics, the initial symptoms and the degree of disability the person experiences as time advances. Life expectancy of people with MS is 5 to 10 years lower than that of the unaffected population.
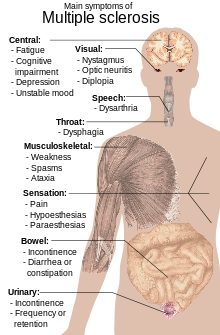
Signs and symptoms
A person with MS can suffer almost any neurological symptom or sign, including changes in sensation such as loss of sensitivity or tingling, pricking or numbness ( hypoesthesia and paresthesia), muscle weakness, clonus, muscle spasms, or difficulty in moving; difficulties with coordination and balance ( ataxia); problems in speech ( dysarthria) or swallowing ( dysphagia), visual problems ( nystagmus, optic neuritis including phosphenes, or diplopia), fatigue, acute or chronic pain, and bladder and bowel difficulties. Cognitive impairment of varying degrees and emotional symptoms of depression or unstable mood are also common. Uhthoff's phenomenon, an exacerbation of extant symptoms due to an exposure to higher than usual ambient temperatures, and Lhermitte's sign, an electrical sensation that runs down the back when bending the neck, are particularly characteristic of MS although not specific. The main clinical measure of disability progression and symptom severity is the Expanded Disability Status Scale or EDSS.
Symptoms of MS usually appear in episodic acute periods of worsening (called relapses, exacerbations, bouts, attacks, or "flare-ups"), in a gradually progressive deterioration of neurologic function, or in a combination of both. Multiple sclerosis relapses are often unpredictable, occurring without warning and without obvious inciting factors with a rate rarely above one and a half per year. Some attacks, however, are preceded by common triggers. Relapses occur more frequently during spring and summer. Viral infections such as the common cold, influenza, or gastroenteritis increase the risk of relapse. Stress may also trigger an attack. Pregnancy affects the susceptibility to relapse, with a lower relapse rate at each trimester of gestation. During the first few months after delivery, however, the risk of relapse is increased. Overall, pregnancy does not seem to influence long-term disability. Many potential triggers have been examined and found not to influence MS relapse rates. There is no evidence that vaccination and breast feeding, physical trauma, or Uhthoff's phenomenon are relapse triggers.
Causes
Most likely MS occurs as a result of some combination of genetic, environmental and infectious factors, and possibly other factors like vascular problems. Epidemiological studies of MS have provided hints on possible causes for the disease. Theories try to combine the known data into plausible explanations, but none has proved definitive.
Genetics
MS is not considered a hereditary disease. However, a number of genetic variations have been shown to increase the risk of developing the disease.
The risk of acquiring MS is higher in relatives of a person with the disease than in the general population, especially in the case of siblings, parents, and children. The disease has an overall familial recurrence rate of 20%. In the case of monozygotic twins, concordance occurs only in about 35% of cases, while it goes down to around 5% in the case of siblings and even lower in half-siblings. This indicates susceptibility is partly polygenically driven. It seems to be more common in some ethnic groups than others.
Apart from familial studies, specific genes have been linked with MS. Differences in the human leukocyte antigen (HLA) system—a group of genes in chromosome 6 that serves as the major histocompatibility complex (MHC) in humans—increase the probability of suffering MS. The most consistent finding is the association between multiple sclerosis and alleles of the MHC defined as DR15 and DQ6. Other loci have shown a protective effect, such as HLA-C554 and HLA-DRB1*11.
Environmental factors
Different environmental factors, both of infectious and non-infectious origin, have been proposed as risk factors for MS. Although some are partly modifiable, only further research—especially clinical trials—will reveal whether their elimination can help prevent MS.
MS is more common in people who live farther from the equator, although many exceptions exist. Decreased sunlight exposure has been linked with a higher risk of MS. Decreased vitamin D production and intake has been the main biological mechanism used to explain the higher risk among those less exposed to sun.
Severe stress may be a risk factor although evidence is weak. Smoking has also been shown to be an independent risk factor for developing MS. Association with occupational exposures and toxins—mainly solvents—has been evaluated, but no clear conclusions have been reached. Vaccinations were investigated as causal factors for the disease; however, most studies show no association between MS and vaccines. Several other possible risk factors, such as diet and hormone intake, have been investigated; however, evidence on their relation with the disease is "sparse and unpersuasive".
Gout occurs less than would statistically be expected in people with MS, and low levels of uric acid have been found in people with MS as compared to normal individuals. This led to the theory that uric acid protects against MS, although its exact importance remains unknown.
Infections
Many microbes have been proposed as potential infectious triggers of MS, but none have been substantiated. Moving at an early age from one location in the world to another alters a person's subsequent risk of MS. An explanation for this could be that some kind of infection, produced by a widespread microbe rather than a rare pathogen, is the origin of the disease. There are a number of proposed mechanisms, including the hygiene hypothesis and the prevalence hypothesis. The hygiene hypothesis proposes that exposure to several infectious agents early in life is protective against MS, the disease being a response to a later encounter with such agents. The prevalence hypothesis proposes that the disease is due to a pathogen more common in regions of high MS prevalence where in most individuals it causes an asymptomatic persistent infection. Only in a few cases and after many years does it cause demyelination. The hygiene hypothesis has received more support than the prevalence hypothesis.
Evidence for viruses as a cause includes the presence of oligoclonal bands in the brain and cerebrospinal fluid of most people with MS, the association of several viruses with human demyelination encephalomyelitis, and induction of demyelination in animals through viral infection. Human herpes viruses are a candidate group of viruses linked to MS. Individuals who have never been infected by the Epstein-Barr virus have a reduced risk of having the disease, and those infected as young adults have a greater risk than those who had it at a younger age. Although some consider that this goes against the hygiene hypothesis, since the noninfected have probably experienced a more hygienic upbringing, others believe that there is no contradiction since it is a first encounter at a later moment with the causative virus that is the trigger for the disease. Other diseases that have also been related with MS are measles, mumps, and rubella.
Pathophysiology
Autoimmunology
MS is believed to be an immune-mediated disorder mediated by a complex interaction of the individual's genetics and as yet unidentified environmental insults. Damage is believed to be caused by the person's own immune system attacking the nervous system. Possible targets of the immune response include myelin basic protein (MBP) and proteolipid protein (PLP). The commonly prescribed MS drug Copaxone was designed to mimic MBP and therefore act as a decoy for autoreactive immune cells. Even so, the role of MBP in MS is controversial; it is buried within the myelin sheath (rather than on the surface), where immune cells would not be able to recognize it.
Recent data suggest a role for myelin lipids in MS. Historically, researchers have assumed the myelin target was a protein, even though the myelin sheath is nearly 80% lipid. Furthermore, lipids are known to be the target of another prominent nervous system autoimmune condition, Guillain-Barre Syndrome.
Whether the autoantigen is a protein or a lipid, autoimmunity may arise when immune cells recognizing a foreign antigen cross-react with self antigens. This process is known as molecular mimicry.
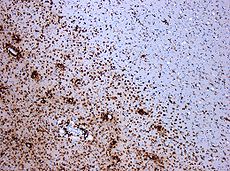
Lesions
The name multiple sclerosis refers to the scars (sclerae – better known as plaques or lesions) that form in the nervous system. MS lesions most commonly involve white matter areas close to the ventricles of the cerebellum, brain stem, basal ganglia and spinal cord; and the optic nerve. The function of white matter cells is to carry signals between grey matter areas, where the processing is done, and the rest of the body. The peripheral nervous system is rarely involved.
More specifically, MS destroys oligodendrocytes, the cells responsible for creating and maintaining a fatty layer—known as the myelin sheath—which helps the neurons carry electrical signals (action potentials). MS results in a thinning or complete loss of myelin and, as the disease advances, the cutting (transection) of the neuron's axons. When the myelin is lost, a neuron can no longer effectively conduct electrical signals. A repair process, called remyelination, takes place in early phases of the disease, but the oligodendrocytes cannot completely rebuild the cell's myelin sheath. Repeated attacks lead to successively fewer effective remyelinations, until a scar-like plaque is built up around the damaged axons. Different lesion patterns have been described.
Inflammation
Apart from demyelination, the other pathologic hallmark of the disease is inflammation. According to a strictly immunological explanation of MS, the inflammatory process is caused by T cells, a kind of lymphocyte. Lymphocytes are cells that play an important role in the body's defenses. In MS, T cells gain entry into the brain via disruptions in the blood–brain barrier. Evidence from animal models also point to a role of B cells in addition to T cells in development of the disease.
The T cells recognize myelin as foreign and attack it as if it were an invading virus. This triggers inflammatory processes, stimulating other immune cells and soluble factors like cytokines and antibodies. Further leaks form in the blood–brain barrier, which in turn cause a number of other damaging effects such as swelling, activation of macrophages, and more activation of cytokines and other destructive proteins.
Blood–brain barrier breakdown
The blood–brain barrier is a part of the capillary system that prevents the entry of T cells into the central nervous system. However, it may become permeable to these types of cells because of an infection or a virus. When the blood–brain barrier regains its integrity, typically after the infection or virus has cleared, the T cells are trapped inside the brain.
Diagnosis
Multiple sclerosis can be difficult to diagnose since its signs and symptoms may be similar to other medical problems. Medical organizations have created diagnostic criteria to ease and standardize the diagnostic process especially in the first stages of the disease. Historically, the Schumacher and Poser criteria were both popular.
Currently, the McDonald criteria focus on a demonstration with clinical, laboratory and radiologic data of the dissemination of MS lesions in time and space for non-invasive MS diagnosis, though some have stated that the only proved diagnosis of MS is autopsy, or occasionally biopsy, where lesions typical of MS can be detected through histopathological techniques.
Clinical data alone may be sufficient for a diagnosis of MS if an individual has suffered separate episodes of neurologic symptoms characteristic of MS. Since some people seek medical attention after only one attack, other testing may hasten and ease the diagnosis. The most commonly used diagnostic tools are neuroimaging, analysis of cerebrospinal fluid and evoked potentials. Magnetic resonance imaging of the brain and spine shows areas of demyelination (lesions or plaques). Gadolinium can be administered intravenously as a contrast to highlight active plaques and, by elimination, demonstrate the existence of historical lesions not associated with symptoms at the moment of the evaluation. Testing of cerebrospinal fluid obtained from a lumbar puncture can provide evidence of chronic inflammation of the central nervous system. The cerebrospinal fluid is tested for oligoclonal bands of IgG on electrophoresis, which are inflammation markers found in 75–85% of people with MS. The nervous system of a person with MS responds less actively to stimulation of the optic nerve and sensory nerves due to demyelination of such pathways. These brain responses can be examined using visual and sensory evoked potentials.
Clinical courses
Several subtypes, or patterns of progression, have been described. Subtypes use the past course of the disease in an attempt to predict the future course. They are important not only for prognosis but also for therapeutic decisions. In 1996 the United States National Multiple Sclerosis Society standardized four clinical courses:
- relapsing remitting,
- secondary progressive,
- primary progressive, and
- progressive relapsing.
The relapsing-remitting subtype is characterized by unpredictable relapses followed by periods of months to years of relative quiet ( remission) with no new signs of disease activity. Deficits suffered during attacks may either resolve or leave sequelae, the latter being more common as a function of time. This describes the initial course of 80% of individuals with MS. When deficits always resolve between attacks, this is sometimes referred to as benign MS, although people will still accrue some degree of disability in the long term. The relapsing-remitting subtype usually begins with a clinically isolated syndrome (CIS). In CIS, a person has an attack suggestive of demyelination, but does not fulfill the criteria for multiple sclerosis. However only 30 to 70% of persons experiencing CIS later develop MS.
Secondary progressive MS describes around 65% of those with an initial relapsing-remitting MS, who then begin to have progressive neurologic decline between acute attacks without any definite periods of remission. Occasional relapses and minor remissions may appear. The median time between disease onset and conversion from relapsing-remitting to secondary progressive MS is 19 years. The primary progressive subtype describes the approximately 10–15% of individuals who never have remission after their initial MS symptoms. It is characterized by progression of disability from onset, with no, or only occasional and minor, remissions and improvements. The age of onset for the primary progressive subtype is later than for the relapsing-remitting, but similar to mean age of progression between the relapsing-remitting and the secondary progressive. In both cases it is around 40 years of age.
Progressive relapsing MS describes those individuals who, from onset, have a steady neurologic decline but also suffer clear superimposed attacks. This is the least common of all subtypes.
Atypical variants of MS with non-standard behaviour have been described; these include Devic's disease, Balo concentric sclerosis, Schilder's diffuse sclerosis and Marburg multiple sclerosis. There is debate on whether they are MS variants or different diseases. Multiple sclerosis also behaves differently in children, taking more time to reach the progressive stage. Nevertheless they still reach it at a lower mean age than adults.
Management
Although there is no known cure for multiple sclerosis, several therapies have proven helpful. The primary aims of therapy are returning function after an attack, preventing new attacks, and preventing disability. As with any medical treatment, medications used in the management of MS have several adverse effects. Alternative treatments are pursued by some people, despite the shortage of supporting, comparable, replicated scientific study.
Acute attacks
During symptomatic attacks, administration of high doses of intravenous corticosteroids, such as methylprednisolone, is the routine therapy for acute relapses, while oral corticosteroids seem to have a similar efficacy and safety profile. Although generally effective in the short term for relieving symptoms, corticosteroid treatments do not appear to have a significant impact on long-term recovery. Consequences of severe attacks which do not respond to corticosteroids might be treated by plasmapheresis.
Disease-modifying treatments
As of January 2013, seven disease-modifying treatments have been approved by regulatory agencies of different countries, including the U.S. Food and Drug Administration (FDA), the European Medicines Agency (EMA) and the Japanese PMDA. The approved drugs are interferon beta-1a, interferon beta-1b, glatiramer acetate, mitoxantrone (an immunosuppressant also used in cancer chemotherapy), natalizumab (a humanized monoclonal antibody immunomodulator), fingolimod and teriflunomide.
The interferons and glatiramer acetate are delivered by frequent injections, varying from once-per-day for glatiramer acetate to once-per-week (but intra-muscular) for interferon beta-1a. Natalizumab and mitoxantrone are given by intravenous (IV) infusion at monthly intervals in the case of natalizumab and every three months in the case of mitoxantrone. In 2010 fingolimod became the first oral drug approved by the FDA, being followed in 2012 by teriflunomide. Fingolimod and teriflunomide are taken through a daily single dose.
Most drugs are approved only for the relapsing-remitting course (RRMS). Medications are modestly effective at decreasing the number of attacks in RRMS.
Interferons and glatiramer acetate are roughly equivalent, reducing relapses by approximately 30%. Comparisons to natalizumab show that the most effective is the latter, both in terms of relapse rate reduction and halting disability progression. Mitoxantrone may be the most effective of them all; however, it is generally not considered as a long-term therapy, as its use is limited by severe secondary effects. While more studies of the long-term effects of the drugs are needed, specially for the newest treatments, existing data on the effects of interferons and glatiramer acetate indicate that early-initiated long-term therapy is safe and it is related to better outcomes.
The earliest clinical presentation of RRMS is the clinically isolated syndrome (CIS). Treatment with interferons during an initial attack decreases the chance that a person will develop clinical MS. Treatment of progressive MS is more difficult than relapsing-remitting MS. Mitoxantrone has shown positive effects in those with secondary progressive and progressive relapsing courses. It is moderately effective in reducing the progression of the disease and the frequency of relapses in short-term follow-up. No treatment has been proven to modify the course of primary progressive MS. Efficacy of most common treatments, interferons and glatiramer acetate, in early-onset MS (before eighteen years of age) has been estimated to be roughly equivalent to adults.
As with many medical treatments, these treatments have several adverse effects. One of the most common is irritation at the injection site for glatiramer acetate and the interferon treatments. Over time, a visible dent at the injection site, due to the local destruction of fat tissue, known as lipoatrophy, may develop. Interferons produce symptoms similar to influenza; some people taking glatiramer experience a post-injection reaction manifested by flushing, chest tightness, heart palpitations, breathlessness, and anxiety, which usually lasts less than thirty minutes. More dangerous but much less common are liver damage from interferons, severe cardiotoxicity, infertility, and acute myeloid leukemia of mitoxantrone, and the putative link between natalizumab and some cases of progressive multifocal leukoencephalopathy. Fingolimod side effects in clinical trials have included cardiovascular conditions, macular edema, infections, liver toxicity and malignancies.
Management of the effects of MS
Disease-modifying treatments reduce the progression rate of the disease, but do not stop it. As multiple sclerosis progresses, the symptomatology tends to increase. The disease is associated with a variety of symptoms and functional deficits that result in a range of progressive impairments and disability. Management of these deficits is therefore very important. Both drug therapy and neurorehabilitation have shown to ease the burden of some symptoms, though neither influences disease progression. Some symptoms have a good response to medication, such as unstable bladder and spasticity, while management of many others is much more complicated. As for any person with neurologic deficits, a multidisciplinary approach is key to improving quality of life; however, there are particular difficulties in specifying a 'core team' because people with MS may need help from almost any health profession or service at some point. Multidisciplinary rehabilitation programs increase activity and participation of people with MS but do not influence impairment level. Due to the paucity of randomized controlled studies, there is limited evidence of the overall efficacy of individual therapy disciplines, though there is good evidence that specific approaches, such as exercise, psychology therapies, particularly cognitive behavioural approaches and energy conservation instruction are effective.
Alternative treatments
Many people with MS use complementary and alternative medicine. Depending on the treatments, the evidence is weak or absent. Examples are a dietary regimen, herbal medicine (including the use of medical cannabis), hyperbaric oxygenation and self-infection with hookworm (known generally as helminthic therapy). Helminthic therapy of infection with Trichuris suis ova is under investigation as of 2013, with expected results of a clinical trial in 2014. Preliminary data indicates that it may be safe and clinically useful.
Prognosis
The prognosis (the expected future course of the disease) for a person with multiple sclerosis depends on the subtype of the disease; the individual's sex, age, and initial symptoms; and the degree of disability the person experiences. The disease evolves and advances over decades, 30 being the mean years to death since onset.
Female sex, relapsing-remitting subtype, optic neuritis or sensory symptoms at onset, few attacks in the initial years and especially early age at onset, are associated with a better course.
The life expectancy of people with MS is 5 to 10 years lower than that of unaffected people. Almost 40% of people with MS reach the seventh decade of life. Nevertheless, two-thirds of the deaths in people with MS are directly related to the consequences of the disease. Suicide also has a higher prevalence than in the healthy population, while infections and complications are especially hazardous for the more disabled ones.
Although most people lose the ability to walk before death, 90% are still capable of independent walking at 10 years from onset, and 75% at 15 years.
Epidemiology
Two main measures are used in epidemiological studies: incidence and prevalence. Incidence is the number of new cases per unit of person–time at risk (usually number of new cases per thousand person–years); while prevalence is the total number of cases of the disease in the population at a given time. Prevalence is known to depend not only on incidence, but also on survival rate and migrations of affected people. MS has a prevalence that ranges between 2 and 150 per 100,000 depending on the country or specific population. Studies on populational and geographical patterns of epidemiological measures have been very common in MS, and have led to the proposal of different etiological (causal) theories.
MS usually appears in adults in their thirties but it can also appear in children. The primary progressive subtype is more common in people in their fifties. As with many autoimmune disorders, the disease is more common in women, and the trend may be increasing. The CDC data suggest that MS is three times more common in women than in men in the United States. In children, the sex ratio difference is higher, while in people over fifty, MS affects males and females almost equally.
There is a north-to-south gradient in the northern hemisphere and a south-to-north gradient in the southern hemisphere, with MS being much less common in people living near the equator. Climate, sunlight and intake of vitamin D have been investigated as possible causes of the disease that could explain this latitude gradient. However, there are important exceptions to the north–south pattern and changes in prevalence rates over time; in general, this trend might be disappearing. This indicates that other factors such as environment or genetics have to be taken into account to explain the origin of MS. MS is also more common in regions with northern European populations. But even in regions where MS is common, some ethnic groups are at low risk of developing the disease, including the Samis, Turkmen, Amerindians, Canadian Hutterites, Africans, and New Zealand Māori.
Environmental factors during childhood may play an important role in the development of MS later in life. Several studies of migrants show that if migration occurs before the age of 15, the migrant acquires the new region's susceptibility to MS. If migration takes place after age 15, the migrant retains the susceptibility of his home country. However, the age–geographical risk for developing multiple sclerosis may span a larger timescale. A relationship between season of birth and MS has also been found which lends support to an association with sunlight and vitamin D. For example fewer people with MS are born in November as compared to May.
History
Medical discovery
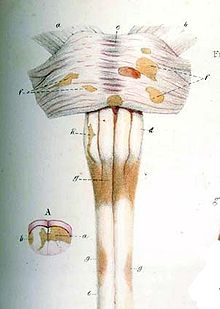
The French neurologist Jean-Martin Charcot (1825–1893) was the first person to recognize multiple sclerosis as a distinct disease in 1868. Summarizing previous reports and adding his own clinical and pathological observations, Charcot called the disease sclerose en plaques. The three signs of MS now known as Charcot's triad 1 are nystagmus, intention tremor, and telegraphic speech (scanning speech), though these are not unique to MS. Charcot also observed cognition changes, describing his patients as having a "marked enfeeblement of the memory" and "conceptions that formed slowly".
Before Charcot, Robert Carswell (1793–1857), a British professor of pathology, and Jean Cruveilhier (1791–1873), a French professor of pathologic anatomy, had described and illustrated many of the disease's clinical details, but did not identify it as a separate disease. Specifically, Carswell described the injuries he found as "a remarkable lesion of the spinal cord accompanied with atrophy". Under the microscope, Swiss pathologist Georg Eduard Rindfleisch (1836–1908) noted in 1863 that the inflammation-associated lesions were distributed around blood vessels.
After Charcot's description, Eugène Devic (1858–1930), Jozsef Balo (1895–1979), Paul Ferdinand Schilder (1886–1940), and Otto Marburg (1874–1948) described special cases of the disease. During all the 20th century there was an important development on the theories about the cause and pathogenesis of MS while efficacious treatments began to appear in 1990.
Historical cases
There are several historical accounts of people who lived before or shortly after the disease was described by Charcot and probably had MS.
A young woman called Halldora who lived in Iceland around 1200 suddenly lost her vision and mobility but, after praying to the saints, recovered them seven days after. Saint Lidwina of Schiedam (1380–1433), a Dutch nun, may be one of the first clearly identifiable MS patients. From the age of 16 until her death at 53, she suffered intermittent pain, weakness of the legs, and vision loss—symptoms typical of MS. Both cases have led to the proposal of a 'Viking gene' hypothesis for the dissemination of the disease.
Augustus Frederick d'Este (1794–1848), son of Prince Augustus Frederick, Duke of Sussex and Lady Augusta Murray and the grandson of George III of the United Kingdom, almost certainly suffered from MS. D'Este left a detailed diary describing his 22 years living with the disease. His diary began in 1822 and ended in 1846, although it remained unknown until 1948. His symptoms began at age 28 with a sudden transient visual loss ( amaurosis fugax) after the funeral of a friend. During the course of his disease, he developed weakness of the legs, clumsiness of the hands, numbness, dizziness, bladder disturbances, and erectile dysfunction. In 1844, he began to use a wheelchair. Despite his illness, he kept an optimistic view of life.
Another early account of MS was kept by the British diarist W. N. P. Barbellion, nom-de-plume of Bruce Frederick Cummings (1889–1919), who maintained a detailed log of his diagnosis and struggle with MS. His diary was published in 1919 as The Journal of a Disappointed Man.
Research
Therapies
Research directions on MS treatments include investigations of MS pathogenesis and heterogeneity; research of more effective, convenient, or tolerable new treatments for RRMS; creation of therapies for the progressive subtypes; neuroprotection strategies; and the search for effective symptomatic treatments. A number of treatments that may curtail attacks or improve function are under investigation. Emerging agents for RRMS that had shown promise in phase 2 trials before 2009 included alemtuzumab, daclizumab, rituximab, dirucotide, BHT-3009, cladribine, dimethyl fumarate, estriol, laquinimod, PEGylated interferon-β-1a, minocycline, statins, temsirolimus and teriflunomide.
Since MS has been related to vitamin D deficiency it has been proposed that vitamin D could be used to treat the disease. Clinical trials have been scarce, of low quality and have not shown clear indication of benefit.
While there is anecdotal evidence of benefit for low dose naltrexone, only results from a pilot study in primary progressive MS have been published.
Disease biomarkers
The variable clinical presentation of MS and the lack of diagnostic laboratory tests lead to delays in diagnosis and the impossibility of predicting diagnosis. New diagnostic methods are being investigated. These include work with anti-myelin antibodies, analysis of microarray gene expression and studies with serum and cerebrospinal fluid but none of them has yielded reliable positive results.
Currently there are no clinically established laboratory investigations available that can predict prognosis. However, several promising approaches have been proposed. Investigations on the prediction of evolution have centered on monitoring disease activity. Disease activation biomarkers include interleukin-6, nitric oxide and nitric oxide synthase, osteopontin, and fetuin-A. On the other hand since disease progression is the result of neurodegeneration the roles of proteins indicative of neuronal, axonal, and glial loss such as neurofilaments, tau and N-acetylaspartate are under investigation.
A final investigative field is work with biomarkers that distinguish between medication responders and nonresponders.
Chronic cerebrospinal venous insufficiency
In 2008, Italian vascular surgeon Paolo Zamboni reported research suggesting that MS involves a vascular disease process he referred to as chronic cerebrospinal venous insufficiency (CCSVI, CCVI), in which veins from the brain are constricted. He found CCSVI in the majority of people with MS, performed a surgical procedure to correct it and claimed that 73% of people improved. Concern has been raised with Zamboni's research as it was neither blinded nor controlled and further studies have had variable results. This has raised serious objections to the hypothesis of CCSVI originating multiple sclerosis. The neurology community currently recommends not to use the proposed treatment unless its effectiveness is confirmed by controlled studies, the need for which has been recognized by the scientific bodies engaged in MS research.