Paracetamol
Did you know...
SOS Children volunteers helped choose articles and made other curriculum material Visit the SOS Children website at http://www.soschildren.org/
 |
|
|---|---|
 |
|
| Systematic (IUPAC) name | |
| N-(4-hydroxyphenyl)ethanamide N-(4-hydroxyphenyl)acetamide |
|
| Clinical data | |
| Trade names | Tylenol (USA), Anacin Aspirin Free (USA), Apra (USA), Crocin (India), Feverall (USA), Genapap (USA), Panadol (UK), Panadol (Australia), Panodil (Denmark), Efferalgan (France), Doliprane (France) Dafalgan (France) |
| AHFS/ Drugs.com | monograph |
| MedlinePlus | a681004 |
| Licence data | US FDA: link |
| Pregnancy cat. | A (AU) B (US) safe |
| Legal status | Unscheduled (AU) GSL (UK) OTC (US) |
| Routes | Oral, rectal, intravenous |
| Pharmacokinetic data | |
| Bioavailability | ~100% |
| Metabolism | 90 to 95% Hepatic |
| Half-life | 1–4 h |
| Excretion | Renal |
| Identifiers | |
| CAS number | 103-90-2 |
| ATC code | N02 BE01 |
| PubChem | CID 1983 |
| DrugBank | DB00316 |
| ChemSpider | 1906 |
| UNII | 362O9ITL9D |
| KEGG | D00217 |
| ChEBI | CHEBI:46195 |
| ChEMBL | CHEMBL112 |
| Chemical data | |
| Formula | C8H9NO2 |
| Mol. mass | 151.17 g/mol |
|
SMILES
|
|
|
InChI
|
|
| Physical data | |
| Density | 1.263 g/cm³ |
| Melt. point | 169 °C (336 °F) |
| Solubility in water | 12.78 mg/mL (20 °C) |
| |
|
Paracetamol INN (pron.: / ˌ p ær ə ˈ s iː t ə m ɒ l / or / ˌ p ær ə ˈ s ɛ t ə m ɒ l /), or acetaminophen USAN / ə ˌ s iː t ə ˈ m ɪ n ə f ɨ n /, chemically named N-acetyl-p-aminophenol, is a widely used over-the-counter analgesic (pain reliever) and antipyretic (fever reducer).
Paracetamol is classified as a mild analgesic. It is commonly used for the relief of headaches and other minor aches and pains and is a major ingredient in numerous cold and flu remedies. In combination with opioid analgesics, paracetamol can also be used in the management of more severe pain such as post-surgical pain and providing palliative care in advanced cancer patients. Though acetaminophen is used to treat inflammatory pain, it is not generally classified as an NSAID because it exhibits only weak anti-inflammatory activity.
The onset of analgesia is approximately 11 minutes after oral administration of paracetamol, and its half-life is 1–4 hours. While generally safe for use at recommended doses (1,000 mg per single dose and up to 4,000 mg per day for adults), acute overdoses of paracetamol can cause potentially fatal kidney, brain and liver damage and, in rare individuals, a normal dose can do the same. The risk may be heightened by chronic alcohol abuse. Paracetamol toxicity is the foremost cause of acute liver failure in the Western world, and accounts for most drug overdoses in the United States, the United Kingdom, Australia and New Zealand.
It is the active metabolite of the coal tar-derived phenacetin, once popular as an analgesic and antipyretic in its own right. However, unlike phenacetin and its combinations, paracetamol is not considered carcinogenic at therapeutic doses. The words acetaminophen (used in the United States, Canada, Japan, South Korea, Hong Kong, and Iran) and paracetamol (used elsewhere) both come from a chemical name for the compound: para-acetylaminophenol and para-acetylaminophenol. In some contexts, it is simply abbreviated as APAP, for acetyl-para-aminophenol.
Medical uses
Fever
Paracetamol is approved for reducing fever in people of all ages. The World Health Organization (WHO) recommends that paracetamol only be used to treat fever in children if their temperature is greater than 38.5 °C (101.3 °F). The efficacy of paracetamol by itself in children with fevers has been questioned and a meta-analysis showed that it is less effective than ibuprofen.
Pain
Paracetamol is used for the relief of pains associated with many parts of the body. It has analgesic properties comparable to those of aspirin, while its anti-inflammatory effects are weaker. It is better tolerated than aspirin in patients in whom excessive gastric acid secretion or prolongation of bleeding time may be a concern. Available without a prescription, it has in recent years increasingly become a common household drug.
Paracetamol can relieve pain in mild arthritis but has no effect on the underlying inflammation, redness, and swelling of the joint. It is as effective as the non-steroidal anti-inflammatory drug ( NSAID) ibuprofen in relieving the pain of osteoarthritis of the knee.
Paracetamol has relatively little anti-inflammatory activity, unlike other common analgesics such as the NSAIDs aspirin and ibuprofen.
Regarding comparative efficacy, studies show conflicting results when compared to NSAIDs. A randomized controlled trial of chronic pain from osteoarthritis in adults found similar benefit from paracetamol and ibuprofen.
The efficacy of paracetamol when used in a combination form with weak opioids (such as codeine) has been questioned by recent data studies; the small amount of data available have made reaching a conclusion difficult. Combination drugs of paracetamol and strong opioids like morphine have been shown to reduce the amount of opioid used and improve analgesic effect as well as discouraging overuse of addictive opioids due to APAP's toxic effects, as it depletes glutathione and thus exacerbates disease in general.
A randomized controlled trial of acute musculoskeletal pain in children found that the standard over-the-counter dose of ibuprofen gives greater pain relief than the standard dose of paracetamol.
Adverse effects
In recommended doses, the side effects of paracetamol are mild to non-existent. In contrast to aspirin, it is not an antithrombotic, and thus may be used in patients where coagulation is a concern, and it does not cause gastric irritation. However, paracetamol does not help reduce inflammation, while aspirin does. Compared to ibuprofen—whose side effects may include diarrhea, vomiting and abdominal pain—paracetamol has fewer adverse gastrointestinal effects. Prolonged daily use increases the risk of upper gastrointestinal complications such as stomach bleeding, and may cause kidney or liver damage. Paracetamol is metabolized by the liver and is hepatotoxic; side effects may be more likely in chronic alcoholics or patients with liver damage.
Until 2010, paracetamol was believed safe in pregnancy (as it does not affect the closure of the fetal ductus arteriosus as NSAIDs can). However, in a study published in October 2010 it has been linked to infertility in the adult life of the unborn. Unlike aspirin, it is safe for children, as paracetamol is not associated with a risk of Reye's syndrome in children with viral illnesses. Paracetamol use for fever in the first year of life was associated with an increase in the incidence of asthmatic symptoms at 6–7 years, and that paracetamol use, both in the first year of life and in children aged 6–7 years, was associated with an increased incidence of rhinoconjunctivitis and eczema. The authors acknowledged that their "findings might have been due to confounding by indication", i.e., that the association may not be causal but rather due to the disease being treated with paracetamol, and emphasized that further research is needed. Furthermore, a number of editorials, comments, correspondence, and their replies have been published in The Lancet concerning the methodology and conclusions of this study. The UK regulatory body the Medicines and Healthcare products Regulatory Agency, also reviewed this research and published a number of concerns over data interpretation, and offer the following advice for healthcare professionals, parents, and care-givers: "The results of this new study do not necessitate any change to the current guidance for use in children. Paracetamol remains a safe and appropriate choice of analgesic in children. There is insufficient evidence from this research to change guidance regarding the use of antipyretics in children. "
Chronic users of paracetamol may have a higher risk of developing blood cancer.
Overdose
Paracetamol hepatotoxicity is, by far, the most common cause of acute liver failure in both the United States and the United Kingdom. Toxicity of paracetamol arises often due to its quinone metabolite. Paracetamol overdose results in more calls to poison control centers in the US than overdose of any other pharmacological substance. Signs and symptoms of paracetamol toxicity may initially be absent or vague. Untreated overdose can lead to liver failure and death within days. Treatment is aimed at removing the paracetamol from the body and replacing glutathione. Activated charcoal can be used to decrease absorption of paracetamol if the patient presents for treatment soon after the overdose. While the antidote, acetylcysteine, (also called N-acetylcysteine or NAC) acts as a precursor for glutathione, helping the body regenerate enough to prevent damage to the liver, a liver transplant is often required if damage to the liver becomes severe. N-Acetylcysteine also helps in neutralizing the imidoquinone metabolite of acetaminophen. Renal failure is also a possible side effect.
There are tablets available (brand-name in the UK Paradote) that combine paracetamol with an antidote ( methionine), to protect the liver in case of an overdose.
In June 2009, a U.S. Food and Drug Administration (FDA) advisory committee recommended that new restrictions should be placed on paracetamol usage in the United States to help protect people from the potential toxic effects. The maximum dosage at any given time would be decreased from 1000 mg to 650 mg, while combinations of paracetamol and narcotic analgesics would be prohibited. Committee members were particularly concerned by the fact that the present maximum dosages of paracetamol had been shown to produce alterations in hepatic function. On January 13, 2011, the FDA asked manufacturers of prescription combination products containing paracetamol to limit the amount of paracetamol to no more than 325 mg per tablet or capsule and began requiring manufacturers to update the labels of all prescription combination paracetamol products to warn of the potential risk for severe liver damage. Manufacturers will have three years to limit the amount of paracetamol in their prescription drug products to 325 mg per dosage unit. In November 2011, the Medicines and Healthcare products Regulatory Agency revised UK dosing of liquid paracetamol for children.
Classification
Paracetamol is part of the class of drugs known as " aniline analgesics"; it is the only such drug still in use today. It is not considered an NSAID because it does not exhibit significant anti-inflammatory activity (it is a weak COX inhibitor). This is despite the evidence that paracetamol and NSAIDs have some similar pharmacological activity.
Mechanism of action
To date, the mechanism of action of paracetamol is not completely understood. The main mechanism proposed is the inhibition of cyclooxygenase (COX), and recent findings suggest that it is highly selective for COX-2. While it has analgesic and antipyretic properties comparable to those of aspirin or other NSAIDs, its peripheral anti-inflammatory activity is usually limited by several factors, one of which is the high level of peroxides present in inflammatory lesions. However, in some circumstances, even peripheral anti-inflammatory activity comparable to NSAIDs can be observed. An article in Nature Communications from researchers in London, UK and Lund, Sweden in November 2011 has found a hint to the analgesic mechanism of paracetamol (acetaminophen), being that the metabolites of paracetamol e.g. NAPQI, act on TRPA1-receptors in the spinal cord to suppress the signal transduction from the superficial layers of the dorsal horn, to alleviate pain. This conclusion has been contested in a new hypothesis paper on how paracetamol might act. The author concedes that NAPQI is the active metabolite but that this reactive compound should react not only with the thiol in TRPA1 but also with any other suitably available nucleophile that it happens to encounter. It is suggested that thiol groups in cysteine proteases, e.g. the proteases that take part in the processing of procytokines, such as those generating IL-1β and IL-6, might be the targets giving rise to overall analgesic effects.
Because of its selectivity for COX-2 it does not significantly inhibit the production of the pro-clotting thromboxanes.
The COX family of enzymes are responsible for the metabolism of arachidonic acid to prostaglandin H2, an unstable molecule that is, in turn, converted to numerous other pro-inflammatory compounds. Classical anti-inflammatories such as the NSAIDs block this step. Only when appropriately oxidized is the COX enzyme highly active.
Paracetamol reduces the oxidized form of the COX enzyme, preventing it from forming pro-inflammatory chemicals. This leads to a reduced amount of prostaglandin E2 in the CNS, thus lowering the hypothalamic set-point in the thermoregulatory centre.
Paracetamol also modulates the endogenous cannabinoid system. Paracetamol is metabolized to AM404, a compound with several actions; what is most important is that it inhibits the reuptake of the endogenous cannabinoid/vanilloid anandamide by neurons. Anandamide reuptake would result in lower synaptic levels and less activation of the main pain receptor (nociceptor) of the body, the TRPV1 (older name: vanilloid receptor). By inhibiting anandamide reuptake, levels in the synapse remain high and are able to desensitize the TRPV1 receptor much like capsaicin. Furthermore, AM404 inhibits sodium channels, as do the anesthetics lidocaine and procaine. Either of these actions by themselves has been shown to reduce pain, and are a possible mechanism for paracetamol. However, it has been demonstrated that, after blocking cannabinoid receptors with synthetic antagonists, paracetamol's analgesic effects are prevented, suggesting its pain-relieving action involves the endogenous cannabinoid system. Spinal TRPA1 receptors have also been demonstrated to mediate antinociceptive effects of paracetamol and Δ9-tetrahydrocannabiorcol in mice.
Aspirin is known to inhibit the cyclooxygenase (COX) family of enzymes and, because paracetamol's action is partially similar to aspirin's, much research has focused on whether paracetamol also inhibits COX. It is now clear that paracetamol acts via at least two pathways.
The exact mechanisms by which COX is inhibited in various circumstances are still a subject of discussion. Because of differences in the activity of paracetamol, aspirin, and other NSAIDs, it has been postulated that further COX variants may exist. One theory holds that paracetamol works by inhibiting the COX-3 isoform - a COX-1 splice variant - of the COX family of enzymes. When expressed in dogs, this enzyme shares a strong similarity to the other COX enzymes, produces pro-inflammatory chemicals, and is selectively inhibited by paracetamol. However, some research has suggested that, in humans and mice, the COX-3 enzyme is without inflammatory action and paracetamol's blockage of it is not significant in its functioning in humans. Another possibility is that paracetamol blocks cyclooxygenase (as in aspirin), but that, in an inflammatory environment where the concentration of peroxides is high, the high oxidation state of paracetamol prevents its actions. This idea would mean that paracetamol has no direct effect at the site of inflammation, but instead acts in the CNS where the environment is not oxidative, to reduce temperature, etc. The exact mechanism by which paracetamol is believed to affect COX-3 is disputed.
Structure and reactivity
Paracetamol consists of a benzene ring core, substituted by one hydroxyl group and the nitrogen atom of an amide group in the para (1,4) pattern. The amide group is acetamide (ethanamide). It is an extensively conjugated system, as the lone pair on the hydroxyl oxygen, the benzene pi cloud, the nitrogen lone pair, the p orbital on the carbonyl carbon, and the lone pair on the carbonyl oxygen are all conjugated. The presence of two activating groups also make the benzene ring highly reactive toward electrophilic aromatic substitution. As the substituents are ortho, para-directing and para with respect to each other, all positions on the ring are more or less equally activated. The conjugation also greatly reduces the basicity of the oxygens and the nitrogen, while making the hydroxyl acidic through delocalisation of charge developed on the phenoxide anion.
Synthesis
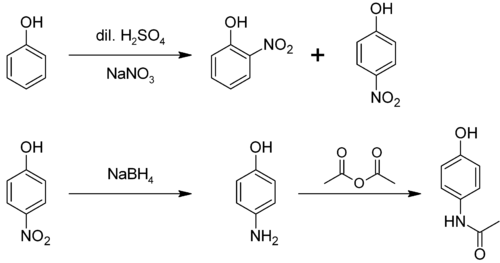
In the laboratory, paracetamol is easily prepared by nitrating phenol with sodium nitrate, separating the desired para- nitrophenol from the ortho- byproduct, and reducing the nitro group with sodium borohydride. The resultant 4-aminophenol is then acetylated with acetic anhydride. In this reaction, phenol is strongly activating, thus the reaction requires only mild conditions (cf. the nitration of benzene). The industrial process is analogous, but hydrogenation is used instead of the sodium borohydride reduction.
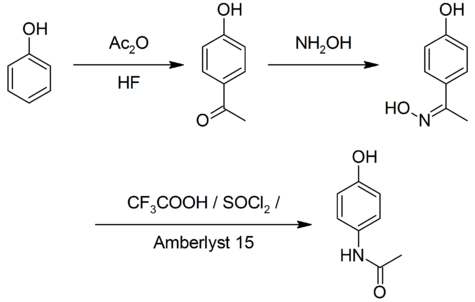
A simpler synthesis by Hoechst-Celanese involves direct acylation of phenol with acetic anhydride catalyzed by HF, conversion of the ketone to a ketoxime with hydroxylamine, followed by the acid-catalyzed Beckmann rearrangement to give the amide.
Demand for paracetamol in the United States was estimated at 30–35 thousand tonnes per year in 1997, equal to the demand from the rest of the world.
Metabolism
Paracetamol is metabolised primarily in the liver, into toxic and non-toxic products. Three metabolic pathways are notable:
- Glucuronidation is believed to account for 40% to two-thirds of the metabolism of paracetamol.
- Sulfation (sulfate conjugation) may account for 20–40%.
- N-hydroxylation and rearrangement, then GSH conjugation, accounts for less than 15%. The hepatic cytochrome P450 enzyme system metabolizes paracetamol, forming a minor yet significant alkylating metabolite known as NAPQI (N-acetyl-p-benzo-quinone imine)(also known as N-acetylimidoquinone). NAPQI is then irreversibly conjugated with the sulfhydryl groups of glutathione.
All three pathways yield final products that are inactive, non-toxic, and eventually excreted by the kidneys. In the third pathway, however, the intermediate product NAPQI is toxic. NAPQI is primarily responsible for the toxic effects of paracetamol; this constitutes an example of toxication.
Production of NAPQI is due primarily to two isoenzymes of cytochrome P450: CYP2E1 and CYP1A2. The P450 gene is highly polymorphic, however, and individual differences in paracetamol toxicity are believed due to a third isoenzyme, CYP2D6. Genetic polymorphisms in CYP2D6 may contribute to significantly different rates of production of NAPQI. Furthermore, individuals can be classified as "extensive", "ultrarapid", "intermediate" and "poor" metabolizers (producers of NAPQI), depending on their levels of CYP2D6 expression. Although CYP2D6 metabolises paracetamol into NAPQI to a lesser extent than other P450 enzymes, its activity may contribute to paracetamol toxicity in extensive and ultrarapid metabolisers, and when paracetamol is taken at very large doses. At usual doses, NAPQI is quickly detoxified by conjugation with glutathione. Following overdose, and possibly also in extensive and ultrarapid metabolizers, this detoxification pathway becomes saturated, and, as a consequence, NAPQI accumulates causing liver and renal toxicity.
Reactions
4-Aminophenol may be obtained by the amide hydrolysis of paracetamol. 4-Aminophenol prepared this way, and related to the commercially available Metol, has been used as a developer in photography by hobbyists. This reaction is also used to determine paracetamol in urine samples: After hydrolysis with hydrochloric acid, 4-aminophenol reacts in ammonia solution with a phenol derivate, e.g. salicylic acid, to form an indophenol dye under oxidization by air.
History
Acetanilide was the first aniline derivative serendipitously found to possess analgesic as well as antipyretic properties, and was quickly introduced into medical practice under the name of Antifebrin by A. Cahn and P. Hepp in 1886. But its unacceptable toxic effects, the most alarming being cyanosis due to methemoglobinemia, prompted the search for less toxic aniline derivatives. Harmon Northrop Morse had already synthesized paracetamol at Johns Hopkins University via the reduction of p-nitrophenol with tin in glacial acetic acid in 1877, but it was not until 1887 that clinical pharmacologist Joseph von Mering tried paracetamol on patients. In 1893, von Mering published a paper reporting on the clinical results of paracetamol with phenacetin, another aniline derivative. Von Mering claimed that, unlike phenacetin, paracetamol had a slight tendency to produce methemoglobinemia. Paracetamol was then quickly discarded in favour of phenacetin. The sales of phenacetin established Bayer as a leading pharmaceutical company. Overshadowed in part by aspirin, introduced into medicine by Heinrich Dreser in 1899, phenacetin was popular for many decades, particularly in widely advertised over-the-counter "headache mixtures", usually containing phenacetin, an aminopyrine derivative of aspirin, caffeine, and sometimes a barbiturate.
Von Mering's claims remained essentially unchallenged for half a century, until two teams of researchers from the United States analyzed the metabolism of acetanilide and paracetamol. In 1947 David Lester and Leon Greenberg found strong evidence that paracetamol was a major metabolite of acetanilide in human blood, and in a subsequent study they reported that large doses of paracetamol given to albino rats did not cause methemoglobinemia. In three papers published in the September 1948 issue of the Journal of Pharmacology and Experimental Therapeutics, Bernard Brodie, Julius Axelrod and Frederick Flinn confirmed using more specific methods that paracetamol was the major metabolite of acetanilide in human blood, and established that it was just as efficacious an analgesic as its precursor. They also suggested that methemoglobinemia is produced in humans mainly by another metabolite, phenylhydroxylamine. A follow-up paper by Brodie and Axelrod in 1949 established that phenacetin was also metabolized to paracetamol. This led to a "rediscovery" of paracetamol. It has been suggested that contamination of paracetamol with 4-aminophenol, the substance von Mering synthesized it from, may be the cause for his spurious findings.
Paracetamol was first marketed in the United States in 1953 by Sterling-Winthrop Co., which promoted it as preferable to aspirin since it was safe to take for children and people with ulcers. The best known brand today for paracetamol in the United States, Tylenol, was established in 1955 when McNeil Laboratories started selling paracetamol as a pain and fever reliever for children, under the brand name Tylenol Children's Elixir—the word "tylenol" was a contraction of para-acetylaminophenol. In 1956, 500 mg tablets of paracetamol went on sale in the United Kingdom under the trade name Panadol, produced by Frederick Stearns & Co, a subsidiary of Sterling Drug Inc. Panadol was originally available only by prescription, for the relief of pain and fever, and was advertised as being "gentle to the stomach," since other analgesic agents of the time contained aspirin, a known stomach irritant. In 1963, paracetamol was added to the British Pharmacopoeia, and has gained popularity since then as an analgesic agent with few side-effects and little interaction with other pharmaceutical agents. Concerns about paracetamol's safety delayed its widespread acceptance until the 1970s, but in the 1980s paracetamol sales exceeded those of aspirin in many countries, including the United Kingdom. This was accompanied by the commercial demise of phenacetin, blamed as the cause of analgesic nephropathy and hematological toxicity.
The U.S. patent on paracetamol has long expired, and generic versions of the drug are widely available under the Drug Price Competition and Patent Term Restoration Act of 1984, although certain Tylenol preparations were protected until 2007. U.S. patent 6,126,967 filed September 3, 1998 was granted for "Extended release acetaminophen particles".
Available forms
Paracetamol is available in a tablet, capsule, liquid suspension, suppository, intravenous, and intramuscular form. The common adult dose is 500 mg to 1000 mg. The recommended maximum daily dose, for adults, is 4000 mg. In recommended doses, paracetamol is generally safe for children and infants, as well as for adults, although rare cases of acute liver injury have been linked to amounts lower than 2500 mg per day.
Panadol, which is marketed in Africa, Asia, Europe, Central America, and Australasia, is the most widely available brand of paracetamol, sold in over 80 countries. In North America, paracetamol is sold in generic form (usually labeled as acetaminophen) or under a number of trade names, for instance, Tylenol ( McNeil-PPC, Inc.), Anacin-3, Tempra, Datril, and Ofirmev. While there is brand named paracetamol available in the UK (e.g. Panadol), unbranded or generic paracetamol is more commonly sold. Acamol, a brand name for paracetamol produced by Teva Pharmaceutical Industries in Israel, is one of the most widely used drugs in that country. In the Philippines, the largest-selling paracetamol brand is Biogesic, manufactured by the drug giant United Laboratories. Biogesic tablet sales reach nearly a billion units each year in the country alone, not including liquid suspension formats. The brand is also available in most of the ASEAN countries where the drug giant has market presence. In Europe, the most common brands of paracetamol are Efferalgan and Doliprane. In India, the most common brand of paracetamol is Crocin manufactured by Glaxo SmithKline Asia. In Bangladesh the most popular two brand are Napa and Renova manufactured by Beximco Pharma and Opsonin Pharma respectively. In China paracetamol is sold over the counter as Duìyǐxiān'ānjīfēn Piàn (对乙酰氨基酚片). Likewise in Japan it is sold under the name Acetaminophen (アセトアミノフェン Asetoaminofen). In North Korea the DPRK-Swiss joint venture PyongSu Pharma markets the drug as PyongSu Cetamol.
In some formulations, paracetamol is combined with the opioid codeine, sometimes referred to as co-codamol ( BAN). In the United States and Canada, this is marketed under the name of Tylenol #1/2/3/4, which contain 8–10 mg, 15 mg, 30 mg, and 60 mg of codeine, respectively. In the U.S., this combination is available only by prescription, while the lowest-strength preparation is over-the-counter in Canada, and, in other countries, other strengths may be available over the counter. There are generic forms of these combinations as well. In the UK and in many other countries, this combination is marketed under the names of Tylex CD and Panadeine. Other names include Captin, Disprol, Dymadon, Fensum, Hedex, Mexalen, Nofedol, Panocod, Paralen, Pediapirin, Perfalgan, and Solpadeine. Paracetamol is also combined with other opioids such as dihydrocodeine, referred to as co-dydramol ( BAN), oxycodone or hydrocodone, marketed in the U.S. as Percocet and Vicodin, respectively. Another very commonly used analgesic combination includes paracetamol in combination with propoxyphene napsylate, sold under the brand name Darvocet. A combination of paracetamol, codeine, and the calmative doxylamine succinate is marketed as Syndol or Mersyndol. The efficacy of paracetamol/codeine combinations have been questioned by recent research.
Paracetamol is commonly used in multi-ingredient preparations for migraine headache, typically including butalbital and paracetamol with or without caffeine, and sometimes containing codeine.
Veterinary use
Paracetamol is extremely toxic to cats, which lack the necessary glucuronyl transferase enzymes to safely break it down. Initial symptoms include vomiting, salivation, and discolouration of the tongue and gums. Unlike an overdose in humans, liver damage is rarely the cause of death; instead, methemoglobin formation and the production of Heinz bodies in red blood cells inhibit oxygen transport by the blood, causing asphyxiation ( methemoglobemia and hemolytic anaemia). Treatment with N-acetylcysteine, methylene blue or both is sometimes effective after the ingestion of small doses of paracetamol.
Although paracetamol is believed to have no significant anti-inflammatory activity, it has been reported as effective as aspirin in the treatment of musculoskeletal pain in dogs. A paracetamol-codeine product (trade name Pardale-V) licensed for use in dogs is available on veterinary prescription in the UK. It should be administered to dogs only on veterinary advice and with extreme caution. The main effect of toxicity in dogs is liver damage, GI ulceration has been reported. N-acetylcysteine treatment is efficacious in dogs when administered within a 2 hours of paracetamol ingestion.
Paracetamol is also lethal to snakes, and has been suggested as a chemical control program for the invasive brown tree snake (Boiga irregularis) in Guam. Doses of 80 mg are inserted into dead mice scattered by helicopter.